Understanding AIDS: Myths, Realities, and the Road Ahead
AIDS—Acquired Immunodeficiency Syndrome—continues to be a subject of intense public interest, debate, and controversy more than four decades after it was first identified. Its impact has been both deeply personal and profoundly societal, touching millions of lives, challenging health systems, and provoking discussions about science, policy, stigma, and human rights.
In this in-depth article, we’ll explore the current landscape of AIDS; highlight what everyone should know; examine the controversies and common misconceptions; and ponder where we go from here.
What Is AIDS? An Overview
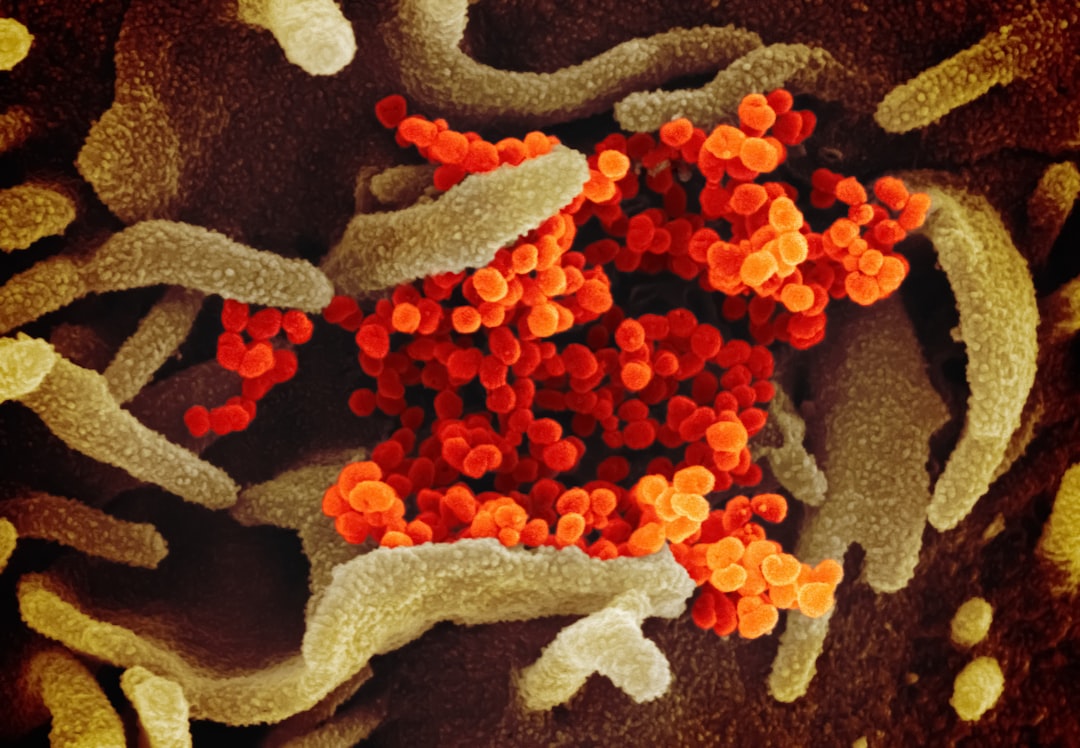
AIDS is a condition caused by the human immunodeficiency virus (HIV). While HIV is the virus, AIDS refers to the advanced stage of infection when the immune system becomes severely weakened.
- HIV Transmission: Through blood, sexual contact, childbirth, or breastfeeding.
- Progression: Without treatment, HIV typically advances to AIDS in 10–15 years. Effective antiretroviral therapy (ART) can prevent this progression and enable those with HIV to live long, healthy lives.
The Impact: Numbers That Matter
Consider these current facts and statistics (2024):
| Metric | Statistic |
|---|---|
| People living with HIV | 39 million globally |
| New HIV infections (2022) | 1.3 million |
| AIDS-related deaths (2022) | 630,000 |
| ART coverage (2022) | 76% of people with HIV |
| Highest prevalence region | Sub-Saharan Africa |
Source: UNAIDS, WHO June 2024
Despite tremendous advances, AIDS remains a global health crisis, especially in low- and middle-income countries.
Myths, Stigma, and Misinformation
Stigma remains one of the most significant barriers to tackling AIDS. Misconceptions about HIV/AIDS fuel discrimination, prevent testing and treatment, and profoundly impact mental health.
Common Myths (and the Truth)
- "HIV is a death sentence."
Fact: With early detection and ART, people with HIV can expect nearly normal lifespans. - "Only certain groups are at risk."
Fact: HIV affects all demographics. While some groups have higher risk, anyone can contract HIV. - "HIV can be transmitted through casual contact."
Fact: Not through hugging, shaking hands, or sharing dishes. - "AIDS can be cured."
Fact: There is currently no cure, but treatment is highly effective.
Hot Debates: Prevention, Criminalization, and Cure
1. Prevention vs. Personal Freedom
Should governments mandate HIV testing for certain populations or leave all testing voluntary? Some argue that mandatory testing can save lives, while others claim it infringes on privacy and human rights.
Debate Points
- Proponents cite public health protection and early intervention.
- Opponents warn of increased stigma, discrimination, and reduced trust in health systems.
2. The Criminalization of HIV Transmission
Some countries criminalize the knowing transmission of HIV. Critics argue that these laws discourage testing and reinforce stigma. Advocates believe they protect people from reckless endangerment.
Provocative Question:
Does the threat of criminal charges empower or undermine public health efforts?
3. The Search for a Cure
Billions spent, decades passed, and no universal cure yet. There have been rare cases of apparent cures—most famously the “Berlin Patient,” Timothy Ray Brown, who was cured via a bone marrow transplant—but these are not scalable solutions.
Future of Cure Research
- Gene editing: CRISPR and similar technologies offer hope, but raise ethical and safety questions.
- Therapeutic vaccines: Long-term promise, but slow progress.
Exploring Prevention: What Really Works?
Tools of Prevention
| Prevention Tool | Effectiveness | Controversy |
|---|---|---|
| Condoms | High | Access/acceptance varies |
| Pre-exposure prophylaxis (PrEP) | Very high | Cost, adherence, access issues |
| Voluntary male circumcision | Moderate | Cultural and religious debates |
| Education | Crucial | Effectiveness tied to social context |
- Needle-exchange programs have proven effective in reducing transmission among injecting drug users, but are controversial in some countries due to perceptions of “enabling” drug use.
Surprising Insight
PrEP—daily medication for high-risk individuals—reduces HIV risk by up to 99%. Yet, uptake remains alarmingly low in parts of the world where it''s needed most, largely due to stigma, access, and cost barriers.
Real-World Stories
Thandiwe’s Journey:
A young woman in South Africa, Thandiwe only learned of her HIV status during a routine pregnancy check. “I thought my life was over,” she says. But with ART and strong community support, she delivered an HIV-negative child and returned to work, becoming an activist for stigma reduction.
Mark’s Challenge:
A gay man in the U.S., Mark faced rejection from friends after disclosing his diagnosis. With therapy and social networks, he rebuilt his life, but wonders: “Why is stigma still so strong—especially when HIV is now so treatable?”
Innovations, Trends, and What’s Next
Current Trends
- Long-acting injectable therapies: Monthly or bimonthly injections replacing daily pills.
- U=U Awareness: “Undetectable = Untransmittable”—when viral load is suppressed, HIV cannot be sexually transmitted.
- Global initiatives: UNAIDS 95-95-95 targets: 95% diagnosed, 95% on treatment, 95% virally suppressed by 2030.
Future Implications
- Wider access to PrEP and ART could dramatically reduce new infections—but only if stigma, cost, and infrastructure issues are addressed.
- Equity challenge: Will low-income regions see the benefits of new treatments, or will disparities widen?
- Will we see a cure in our lifetime? Experts are cautiously optimistic, given unprecedented speed in vaccine and gene therapy innovation.
Challenging Assumptions
Experts urge us to rethink what we know:
- HIV/AIDS is not just a health issue, but a social justice issue.
- Stigma can be as devastating as the virus itself.
- “High-risk” populations are often most underserved, yet bear the brunt of the epidemic.
“The science is there, the meds are there. The real challenge is the will—social, political, and economic—to end AIDS as a public health threat.”
— Dr. Linda-Gail Bekker, Desmond Tutu HIV Centre
Actionable Advice: What Can You Do?
- Get tested: Knowing your status is the first step.
- Fight stigma: Speak up against ignorance and prejudice.
- Stay informed: Misinformation can cost lives.
- Support organizations: Advocacy and education groups make a difference.
Table: Comparing Myths vs. Facts
| Myth | Fact |
|---|---|
| HIV = Death | Lifespan is near normal with treatment |
| HIV only for “others” | Anyone can get HIV |
| Only “immoral” behavior leads to HIV | Many, including monogamous people, are affected |
| Casual touch spreads HIV | Transmission requires certain body fluids |
Conclusion: The Future We Imagine
Have we done enough—or are we letting prejudice and misinformation stall the fight against AIDS? Can we envision a world where no one fears testing, everyone has treatment, and stigma has vanished?
The road ahead merges science and humanity. Will societies rise to the challenge, or will old attitudes persist despite the advancing frontiers of medicine?
What will you do—today, this year, in your community—to build an AIDS-free generation? The answer may define the future far more than the virus itself ever could.
Keywords: AIDS, HIV, stigma, prevention, cure, treatment, myths, facts, PrEP, antiretroviral therapy, HIV transmission, global health, public policy, controversy, health equity, future trends.
Let’s continue this conversation. Share your thoughts below: What surprised you most? Where do you think the greatest challenges—and hopes—lie?