Understanding Psychosis: Causes, Symptoms, Diagnosis, and Treatment
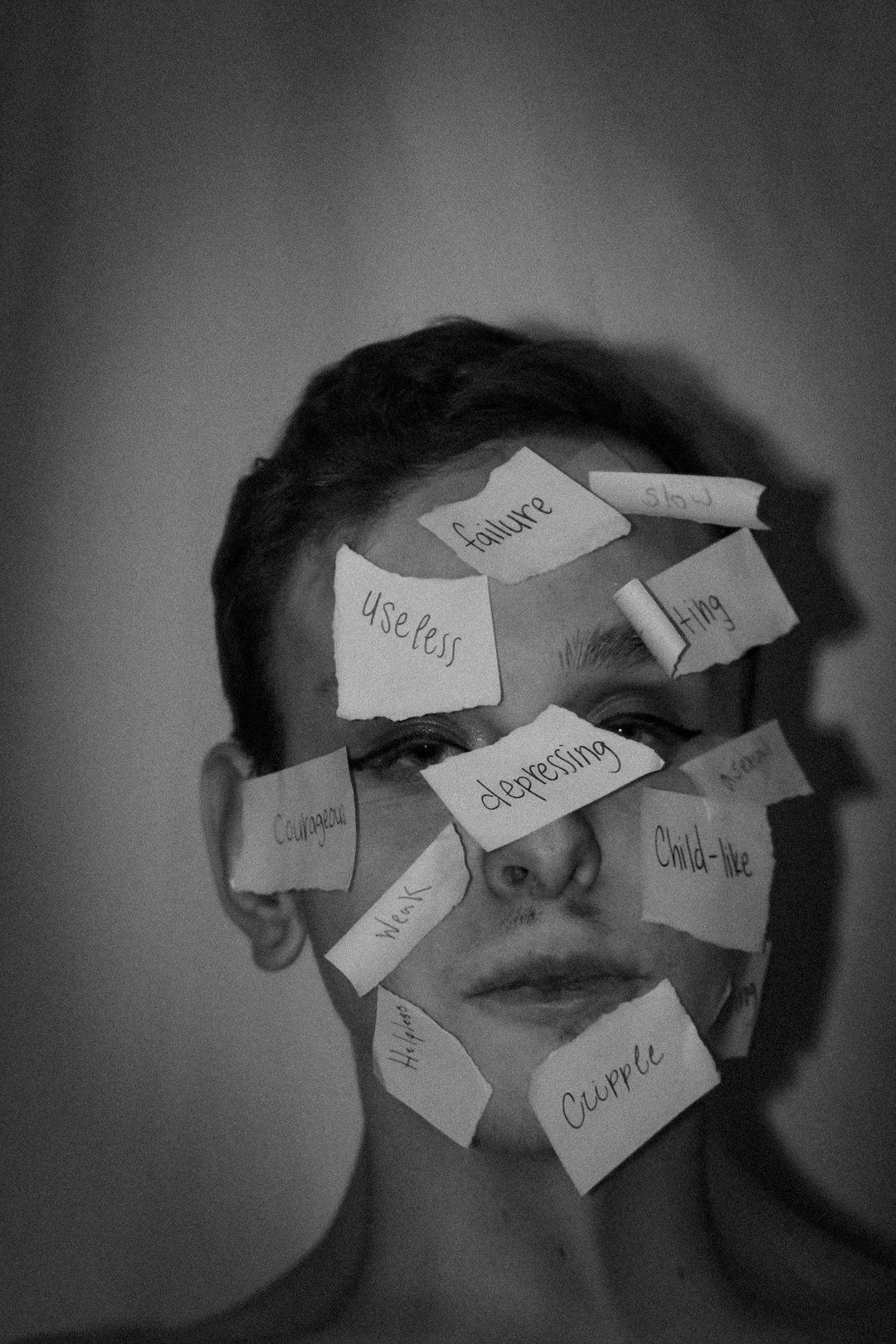
Psychosis refers to a group of mental health symptoms that affects the way a person thinks, perceives, and interprets reality. Often misunderstood and stigmatized, psychosis can have profound impacts on individuals, families, and society. This article delves into the causes, symptoms, diagnosis, and treatment of psychosis, aiming to offer a comprehensive overview of this complex mental health phenomenon.
What is Psychosis?
Psychosis is a condition characterized by an impaired relationship with reality, often involving delusions (false beliefs) and hallucinations (seeing, hearing, or feeling things that are not there). While psychosis can be a one-time event, it may also occur as part of a longer-term psychiatric disorder, such as schizophrenia or bipolar disorder.
Causes of Psychosis
Psychosis can have multiple causes, including biological, psychological, and environmental factors:
| Cause | Description | Examples |
|---|---|---|
| Mental Illness | Primary psychiatric disorders often cause psychotic symptoms | Schizophrenia, Bipolar I Disorder |
| Substance Use | Intoxication or withdrawal from drugs/alcohol can trigger psychosis | LSD, Methamphetamine, Alcohol |
| Medical Conditions | Brain diseases, infection, or injury can cause psychosis | Brain tumor, Dementia, Encephalitis |
| Trauma or Stress | Severe psychological trauma or prolonged stress | PTSD-related psychosis |
| Sleep Deprivation | Extended periods without sleep can induce psychosis | N/A |
| Genetic Factors | Family history increases vulnerability | N/A |
Symptoms of Psychosis
Symptoms are typically divided into positive and negative categories:
| Category | Symptom | Description/Examples |
|---|---|---|
| Positive | Hallucinations | Hearing voices, seeing things not there |
| Positive | Delusions | False beliefs (paranoia, grandiosity, thought insertion, etc.) |
| Positive | Disorganized Thinking | Incoherent speech, trouble concentrating |
| Positive | Disorganized Behavior | Odd or unpredictable actions |
| Negative | Emotional Flatness | Lack of emotional expression |
| Negative | Social Withdrawal | Isolation, loss of interest in activities |
| Negative | Anhedonia | Inability to experience pleasure |
| Negative | Avolition | Decreased motivation to perform everyday tasks |
Note: “Positive” and “negative” refer to the presence (positive) or absence (negative) of behaviors, not value judgments.
Stages of Psychosis
| Stage | Features |
|---|---|
| Prodromal Phase | Subtle changes in thoughts, mood, and social functioning; may last weeks/months |
| Acute Phase | Full-blown psychotic symptoms (hallucinations, delusions, disorganization) |
| Recovery/Residual Phase | Reduction in symptoms; may persist with mild or residual effects |
Diagnosing Psychosis
Diagnosing psychosis involves a combination of clinical interviews, mental status examinations, and, sometimes, laboratory or imaging tests to rule out physical causes.
Common Assessment Tools:
- Structured clinical interviews (e.g., SCID, MINI)
- Mental status examination
- Neuroimaging (MRI, CT) if physical cause is suspected
- Blood and urine tests (screen for metabolic, infectious, or substance-related causes)
Treatment Options
1. Medications
Antipsychotics are the mainstay of psychosis treatment. They are divided into two categories:
| Type | Examples | Key Features/Side Effects |
|---|---|---|
| First Generation | Haloperidol, Chlorpromazine | May cause movement disorders (EPS, tardive dyskinesia) |
| Second Generation | Risperidone, Olanzapine, Quetiapine | Lower risk of movement disorders, may cause weight gain, diabetes |
2. Psychological Therapies
- Cognitive Behavioral Therapy for Psychosis (CBTp): Helps patients challenge and manage distressing thoughts.
- Family Therapy: Reduces relapse and improves outcomes.
- Psychoeducation: For patients and families to understand and manage symptoms.
3. Social and Community Support
- Supported Employment/Education: Assists with reintegration into work or school.
- Case Management: Coordinates care and access to housing, benefits, social support.
4. Hospitalization
May be necessary in cases of severe symptoms, risk to self or others, or inability to care for oneself.
Prognosis and Long-Term Outlook
The outcome for psychosis varies greatly:
| Factor | Impact on Prognosis |
|---|---|
| Early Intervention | Better long-term outcomes |
| Adherence to Treatment | Reduces recurrence/relapse |
| Substance Use | Worsens prognosis |
| Support Networks | Improves outcome |
| Chronicity of Disorder | Some diagnoses (e.g., schizophrenia) may persist lifelong |
Myths and Misconceptions
| Myth | Fact |
|---|---|
| All people with psychosis are violent | Most are not; many are more at risk for self-harm than harming others |
| Psychosis is the same as “psychopathy” | They are distinct; psychosis involves losing touch with reality |
| Medication can “cure” psychosis instantly | Medication manages symptoms, but recovery may take time |
| Only people with mental illness experience it | Physical illness, drugs, and stress can also cause psychosis |
When to Seek Help
Contact a medical or mental health professional if you or someone you know experiences:
- Hearing or seeing things that others don’t
- Persistent, unusual beliefs or paranoia
- Severe confusion, disorganized thinking
- Withdrawal from family, friends, or usual activities
Immediate help is needed if there is a risk of harm to self or others.
Conclusion
Psychosis is a serious but treatable mental health condition. Advances in understanding, diagnosis, and therapy mean that many people can recover or manage their symptoms effectively with the right support. Reducing stigma and increasing awareness remain vital for improving outcomes and quality of life for those affected.
Further Resources
- National Alliance on Mental Illness (NAMI)
- Early Psychosis Intervention Network
- World Health Organization - Schizophrenia and Other Psychoses
Disclaimer: This article is for informational purposes only and not a substitute for professional medical advice, diagnosis, or treatment.